Abstract
Introduction:Anticoagulation (AC) is effective for the treatment of venous thromboembolism (VTE) in cancer patients, but is associated with an increased risk of bleeding. Currently, LMWH monotherapy is the recommended treatment for cancer patients with VTE; however, emerging data from Medicare patients suggests that rivaroxaban had a significantly lower risk of VTE recurrence and similar risk of major bleeding compared to LMWH or warfarin. In this study, we compared the effectiveness and risk of major bleeding associated with these anticoagulants in a younger cohort of patients from a commercial claims database.
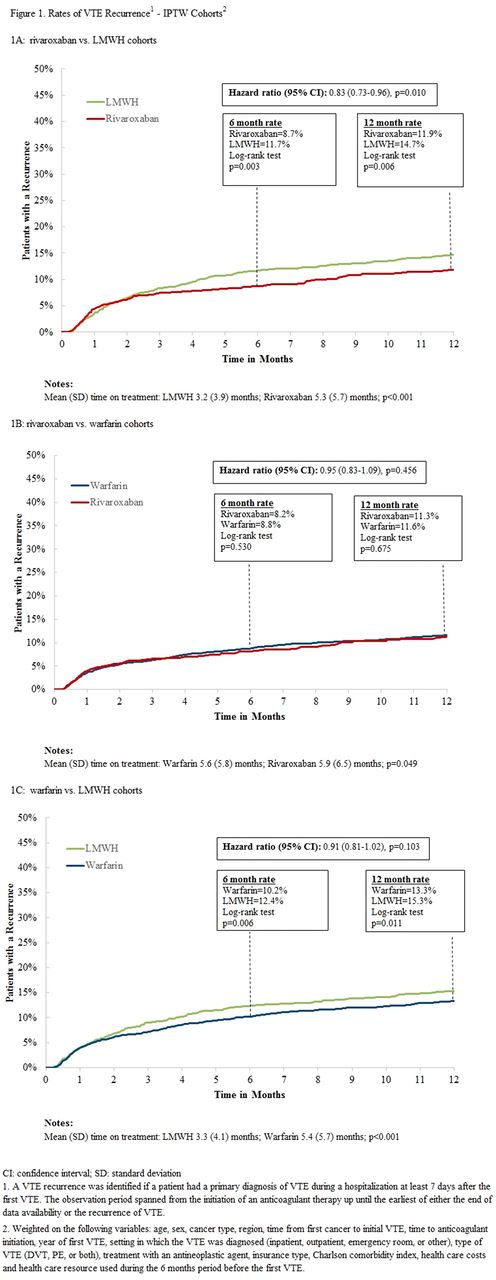
Methods: Truven Health Analytics MarketScan databases were used to find patients aged ≥18 newly diagnosed with cancer who then had their first VTE (deep vein thrombosis (DVT) or pulmonary embolism (PE); excluding upper VTE) between 1/1/2013 - 9/30/2016 and AC start ≤ 7 days. Patients were categorized into LMWH, warfarin, or rivaroxaban cohorts based on index AC. The warfarin cohort included patients who started LMWH and warfarin ≤ 7 days of their first VTE. Inverse probability of treatment weights based on propensity score were used to adjust for treatment differences in the comparison of LMWH vs. rivaroxaban, warfarin vs. rivaroxaban, and LMWH vs. warfarin. Patients were observed until the earliest of end of eligibility or data end. VTE recurrences were defined conservatively as hospitalizations with a primary diagnosis of VTE ≥7 days after the first VTE. Major bleeding events were identified using validated criteria (Cunningham et al., 2011) and evaluated while patients were on treatment. Kaplan-Meier rates at 6 and 12 months were used to compare VTE recurrence between cohorts. Time on treatment was approximately 30-50% of total eligibility time, so rates at 3 and 6 months were used to compare major bleeding between cohorts. Cox proportional hazard models were used to compare VTE recurrence and major bleeding risk between cohorts.
Results: A total of 12,457 patients (LMWH: N=4,313; warfarin; N=4,774; rivaroxaban: N=3,370) were included. After weighting the cohorts, baseline demographic and clinical characteristics were well balanced. Mean patient age ranged from 61.3 to 63.6 years. Median observation time with LMWH was shorter than with rivaroxaban (6.8 vs. 8.3 months, p<0.001) and with warfarin (7.4 vs. 9.8 months, p<0.001). Time on treatment was significantly shorter as well (Figures 1A-1C). VTE recurrence rates were significantly lower with rivaroxaban than with LMWH users at 6 months (8.7% vs. 11.7%; p=0.003) and 12 months (11.9% vs.14.7%; p=0.006), respectively, with a hazard ratio (HR [95%CI]) of 0.83 (0.73-0.96; p=0.010; Figure 1A). Major bleeding rates for rivaroxaban and LMWH users were similar at 3 months (3.2% vs. 3.5%; p=0.592) and 6 months (4.4% vs. 4.9%; p=0.438), respectively [HR 0.91 (0.71-1.17; p=0.455]. VTE recurrence rates for rivaroxaban and warfarin users were similar at 6 months (8.2% vs 8.8%; p=0.530) and 12 months (11.3% vs 11.6%; p=0.675), respectively [HR 0.95 (0.83-1.09; p=0.456; Figure 1B)]. Major bleeding rates for rivaroxaban and warfarin users were also similar at 3 months (3.2% vs. 2.8%; p=0.199) and 6 months (4.2% vs. 3.8%; p=0.362), respectively [HR 1.08 (0.86-1.37; p=0.500)]. Recurrence rates were significantly lower for warfarin users than for LMWH users at 6 months (10.2% vs. 12.4%; p=0.006) and 12 months (13.3% vs. 15.3%; p=0.011), respectively, but the rate of recurrence over the entire follow up was not significantly different between the two cohorts [HR of 0.91 (0.81-1.02; p=0.103; Figure 1C)]. Major bleeding rates for warfarin and LMWH users were similar at 3 months (3.1% vs. 3.7%; p=0.114) and 6 months (4.3% vs. 5.1%; p=0.109), respectively [HR of 0.86 (0.68-1.08; p=0.187)].
Conclusion: In this large cohort of cancer patients treated for VTE, time on treatment was shorter for patients treated with LMWH than oral agents. Rivaroxaban was associated with a significantly lower rate of VTE recurrence than LMWH and a similar rate of VTE recurrence to warfarin; major bleed rates were similar for all. While LMWH has been associated with greater reductions in recurrent VTE compared to warfarin in trials, poor persistence on LMWH in real world settings may explain its lack of comparative effectiveness in this analysis.
Khorana: Bayer: Consultancy, Honoraria; Amgen: Consultancy, Honoraria, Research Funding; Sanofi: Consultancy, Honoraria; Janssen Scientific Affairs, LLC: Consultancy, Honoraria, Research Funding; Leo: Consultancy, Honoraria, Research Funding; Halozyme: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Roche: Consultancy, Honoraria. Milentijevic: Janssen Scientific Affairs, LLC: Employment, Equity Ownership. McCormick: Janssen Scientific Affairs, LLC: Research Funding. Laliberté: Janssen Scientific Affairs, LLC: Research Funding. Crivera: Janssen Scientific Affairs, LLC: Employment, Equity Ownership. Lefebvre: Janssen Scientific Affairs, LLC: Research Funding. Lejeune: Janssen Scientific Affairs, LLC: Research Funding. Rozjabek: Janssen Scientific Affairs, LLC: Other: Fellowship supported by Janssen Scientific Affairs, LLC. Schein: Janssen Scientific Affairs, LLC: Employment, Equity Ownership, Other: Own in excess of $10,000 of J&J stock. Streiff: Roche: Research Funding; CSL Behring: Consultancy, Research Funding; Janssen Scientific Affairs, LLC: Consultancy, Research Funding; Portola: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.